Attention-Deficit/Hyperactivity Disorder (ADHD) is one of the most commonly discussed — and misunderstood — childhood neurodevelopmental conditions today. Many parents search for answers after noticing challenges with attention, impulsivity, emotional regulation, or constant restlessness in their child. With social media, online quizzes, and short videos everywhere, it’s easy to feel overwhelmed or unsure about what ADHD really looks like.
ADHD affects how the brain manages focus, activity levels, and impulse control. These challenges can impact learning, relationships, emotional wellbeing, and family dynamics. Understanding ADHD clearly — without fear, labels, or assumptions — helps parents respond with support instead of self-blame.
This guide explains what ADHD is, common signs parents notice, how it is identified, and the kinds of support that actually help children thrive.
What Is ADHD?
ADHD is a neurodevelopmental condition, meaning it relates to how the brain develops and functions. It is characterised by ongoing patterns of:
- Inattention (difficulty focusing, organising, or completing tasks)
- Hyperactivity (excessive movement or restlessness)
- Impulsivity (acting without thinking, difficulty waiting or regulating responses)
These behaviours must:
- Begin in early childhood
- Persist over time
- Be noticeable in more than one setting (such as home and school)
- Interfere with daily functioning, learning, or social relationships
ADHD is not caused by poor parenting, lack of discipline, or laziness. It is also not something children can simply “grow out of” by trying harder — though symptoms may change as they grow.
Common Signs Parents Notice
Not all children with ADHD look the same. Some are loud and constantly moving; others are quiet, distracted, and overwhelmed internally.
Inattention may include:
- Difficulty following instructions
- Trouble finishing homework or tasks
- Frequently losing items
- Seeming forgetful or easily distracted
Hyperactivity may include:
- Constant fidgeting or movement
- Difficulty staying seated
- Excessive talking
- Appearing driven by a “motor”
Impulsivity may include:
- Interrupting conversations
- Acting without thinking about consequences
- Difficulty waiting turns
- Emotional reactions that feel sudden or intense
A child does not need to show all of these signs to have ADHD.
ADHD vs Normal Childhood Behaviour
All children get distracted. All children have energy. All children act impulsively sometimes.
The difference with ADHD lies in:
- Frequency – it happens often
- Intensity – it’s more disruptive than expected for age
- Impact – it affects learning, relationships, or safety
If behaviours are consistent, occur across environments, and significantly affect daily life, it may be worth looking deeper.
How ADHD Is Identified
There is no single test for ADHD.
Identification usually involves:
- Detailed discussions with parents
- Input from teachers or caregivers
- Behavioural questionnaires
- Observing how long symptoms have been present
- Ruling out other factors such as anxiety, sleep issues, learning difficulties, or sensory challenges
A key principle agreed upon by child-health experts:
ADHD is identified based on functional impact, not just behaviour.
What Actually Helps Children with ADHD
ADHD support works best when it is layered and consistent, not rushed or reactive.
1. Structure and Predictability
- Clear routines
- Visual schedules
- Step-by-step instructions
- Fewer rules, applied consistently
2. Positive Behaviour Support
- Immediate, specific praise
- Clear expectations
- Calm, predictable consequences
- Focusing on effort rather than perfection
3. Parent Guidance
Parents benefit greatly from learning:
- How ADHD affects the brain
- Why traditional discipline often backfires
- How to reduce power struggles and emotional overload
This is not about “fixing” parenting — it’s about aligning responses with how a child’s brain works.
4. School and Learning Support
Children with ADHD often need:
- Movement breaks
- Extra time for tasks
- Organisational help
- Clear, written instructions
Small adjustments can make a big difference.
What About Medication?
Medication is not the first step for every child, especially younger ones.
When used:
- It is part of a broader care plan
- It is monitored carefully
- The goal is to reduce symptom intensity — not change personality
Many children do well with behavioural and environmental support alone, especially when started early.
A Personal Reflection: How This Became Real for Me
When my daughter started school and I began sitting with her to teach lessons, something felt harder than I expected. Focus slipped easily. Frustration built quickly — for both of us. Teaching felt emotionally heavy.
Around the same time, my social media feed was filled with ADHD reels and conversations. The signs felt familiar. Too familiar. Doubt crept in. What if she has ADHD?
So I did what many of us do when uncertainty shows up — I took an online quiz. I answered the questions honestly, thinking of my daughter.
The result surprised me.
It didn’t sound like her.
It sounded like me.
That moment sent me into a deep dive — reading research, understanding how ADHD actually presents, and realising how easily our own attention patterns and regulation struggles can surface while parenting.
It also taught me something important: online quizzes can start reflection, but they don’t replace understanding or professional guidance.
Living With ADHD — For Children and Parents
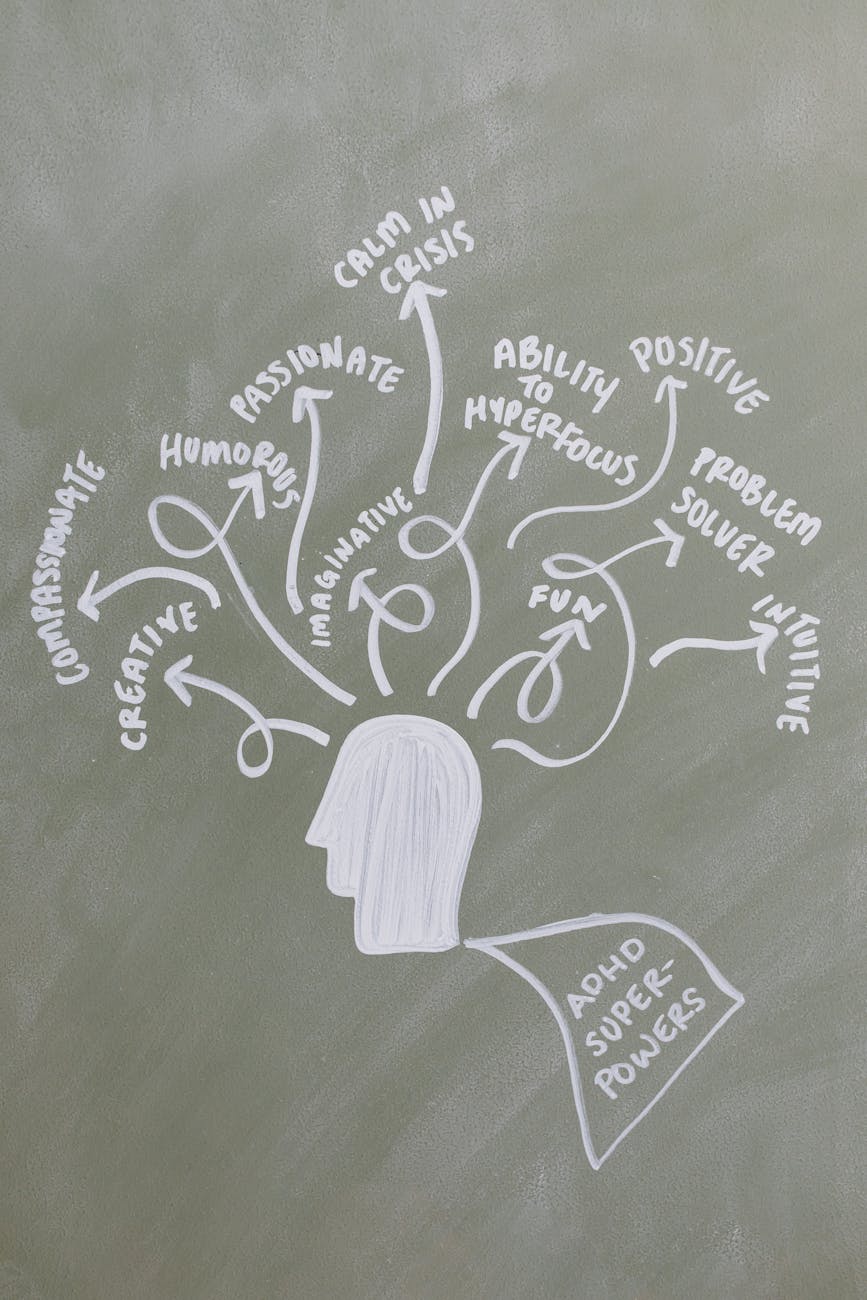
ADHD doesn’t define intelligence, potential, or worth. Many children with ADHD are creative, empathetic, energetic, and deeply curious. With understanding, structure, and support, they can thrive — academically, socially, and emotionally.
Many behaviours we label as “disrespect” are actually struggles with regulation, impulse control, or unmet needs — especially in children with attention challenges.
For parents, learning about ADHD often becomes less about labels and more about compassion — for our children and ourselves.
If you suspect ADHD:
- Pause before self-blame
- Seek accurate information
- Focus on support, not labels
Understanding comes before action — and understanding changes everything.
References & Further Reading
The information in this article is informed by guidance and consensus from leading pediatric and child-health organizations, including:
- American Academy of Pediatrics (AAP)
Attention-Deficit/Hyperactivity Disorder (ADHD): Overview, diagnosis, and management guidelines. - Indian Academy of Pediatrics (IAP)
Parental Guidelines for the Hyperactive Child. - National Institute for Health and Care Excellence (NICE)
Attention deficit hyperactivity disorder: diagnosis and management. - National Health Service (NHS)
Attention deficit hyperactivity disorder (ADHD). - Australian ADHD Professionals Association (AADPA)
Evidence-Based Clinical Practice Guideline for ADHD.
Understanding ADHD involves more than recognizing symptoms — it requires empathy, insight into emotional and behavioral patterns, and effective ways to support your child’s growth. For broader guidance on emotional development, behavior differences, and supporting children through a range of experiences, explore our Emotional Growth & Behavior pillar.



Leave a comment